What would you highlight regarding the barriers in the outreach of harm reduction services based on the findings?
Funding, lack of political will and lack of or insufficient involvement of people who use drugs in services were reported as the main barriers to reaching out to specific subgroups of people who use drugs. Of course, all of these aspects are related to one another. Funding is an evergreen topic which is always there, and the lack of or insufficient funding is a direct consequence of the lack of political will. If there was political support for harm reduction, there would have been funding as well.
Are there any main differences in the availability, accessibility and quality of the services between the cities of the focal points?
On the one hand, we have opioid agonist treatment, needle distribution programs and all of the infectious diseases-related services, such as testing and treatment. These are well-developed in general in terms of availability, accessibility and quality.
On the other hand, there are some more innovative services that maybe, as I said before, are not that much connected, at least in the minds of the general public and the policymakers, with direct prevention of infectious diseases. These services that go beyond the ‘traditional’ harm reduction and focus primarily (but not exclusively) on overdose prevention are the drug consumption rooms (DCRs) and drug checking. These are in general more available in Western European countries. Snorting kits, kits for smoking, and fentanyl strips are also less available and accessible.
There are no DCRs in Central-Eastern Europe and Western Balkans. They are quite well developed as a network in Germany, Switzerland, Spain and maybe two other countries. In some countries, such as Greece or Portugal, there are one or two services. Drug checking is similar. There is a clear division between Central-Eastern Europe and Western Balkans on the one hand and Western Europe on the other, in terms of service scope, service accessibility, low versus high threshold of various services, and the very service existence in the first place.
Harm reduction is chronically underfunded everywhere, but that means something different in the West and in Eastern-Central Europe and Western Balkans. In the East and Southeast, underfunded means that an insufficient number of services are operating or – in extreme cases – they are not funded for several months in a year because there are gaps between grants. Underfunded in the West seems to mean mostly that services don’t have enough funds to develop the offer, scale up activities and broaden their scope. We can also see that in the West, in general, services are more integrated into the health and social care systems, and in the East, they are more standing alone. One of the worrying phenomena that we observed this year, however, is the extremely low availability and accessibility of social integration services, such as housing, income generation and employment, and legal support. Furthermore, for the two latter types of services, we’ve observed significant deterioration in availability over the last couple of years.
We also know from the previous Monitoring edition that there are divisions between the urban and rural areas. Services are focused and concentrated in big cities, and they are lacking in the countryside. The question is also to what extent they are needed in the rural areas, as we also know that the concentration of people who use drugs is also in bigger cities. Some level of services is necessary in rural areas, but what level of availability and accessibility is necessary is something that would require additional assessment.
How do you think that harm reduction organizations can use the report?
We are trying to follow the requests of the Focal Points in terms of the focus and to make our assessments address the topics that are important to people at any given moment.
When it comes to using the report in advocacy efforts, harm reduction organisations can use it to highlight cities and countries that can serve as good practice examples, like Bern or Amsterdam, with holistic, integrated services. The report is a general overview of the situation in Europe, and it can serve as a starting point in orienting oneself in what’s happening in different cities.
In the context of talking to policymakers, the report – in conjunction, for example, with the European Drug Strategy, which calls for scaling up harm reduction services – can help to showcase the gaps in harm reduction services at the city level compared to what is declared by a country or a city in official policy documents. This can potentially be quite a powerful tool in helping organisations in their advocacy efforts.
What do you think is the added value of civil society-led monitoring in comparison with other types of monitoring done by major agencies?
One of the added values is trust and the hands-on experience of our Focal Points, and the related kind and detail of the information collected. Civil society organisations are close to people who use drugs, and people who use drugs trust them enough to share honest information. For example, from the point of view of drug checking, this means that we can have very detailed information on how people use drugs, what drugs they use, in what contexts, etc. This is in sharp contrast, for example, to wastewater analysis that can tell us how much cocaine is in the wastewater but cannot provide information about the people who used it and the circumstances, if they used it at all.
For our monitoring, we collect data in a way that is contextualised. This is quite different from data collected, for example, by the national Reitox focal points that focus on the existence of services and perhaps the number of services.
On the other hand, when we ask to what extent particular types of services are available to specific communities and to what extent they are accessible, we implicitly include the element of the needs. That is this contextualisation of data that I mentioned, which includes additional information. For example, seven services existing in one city can mean something completely different than the same number of services in another city because the needs are different, and this is what we address with our monitoring. This is one of the main values of C-EHRN monitoring compared to other data.
Another point is focus on the city level. Most data is collected by European agencies and country governments is collected at the national level. Our data is collected at the city level, which is important primarily because the implementation of drug policies is done mostly at the local level in European countries.
We are also quite timely with our data. We are now at the beginning of 2024, and we are reporting on the data between 2022 and June 2023, a bit over one year of delay in reporting. This is also something that makes us different, less bureaucracy and resulting quicker data processing give us the possibility of being quicker with our reporting.
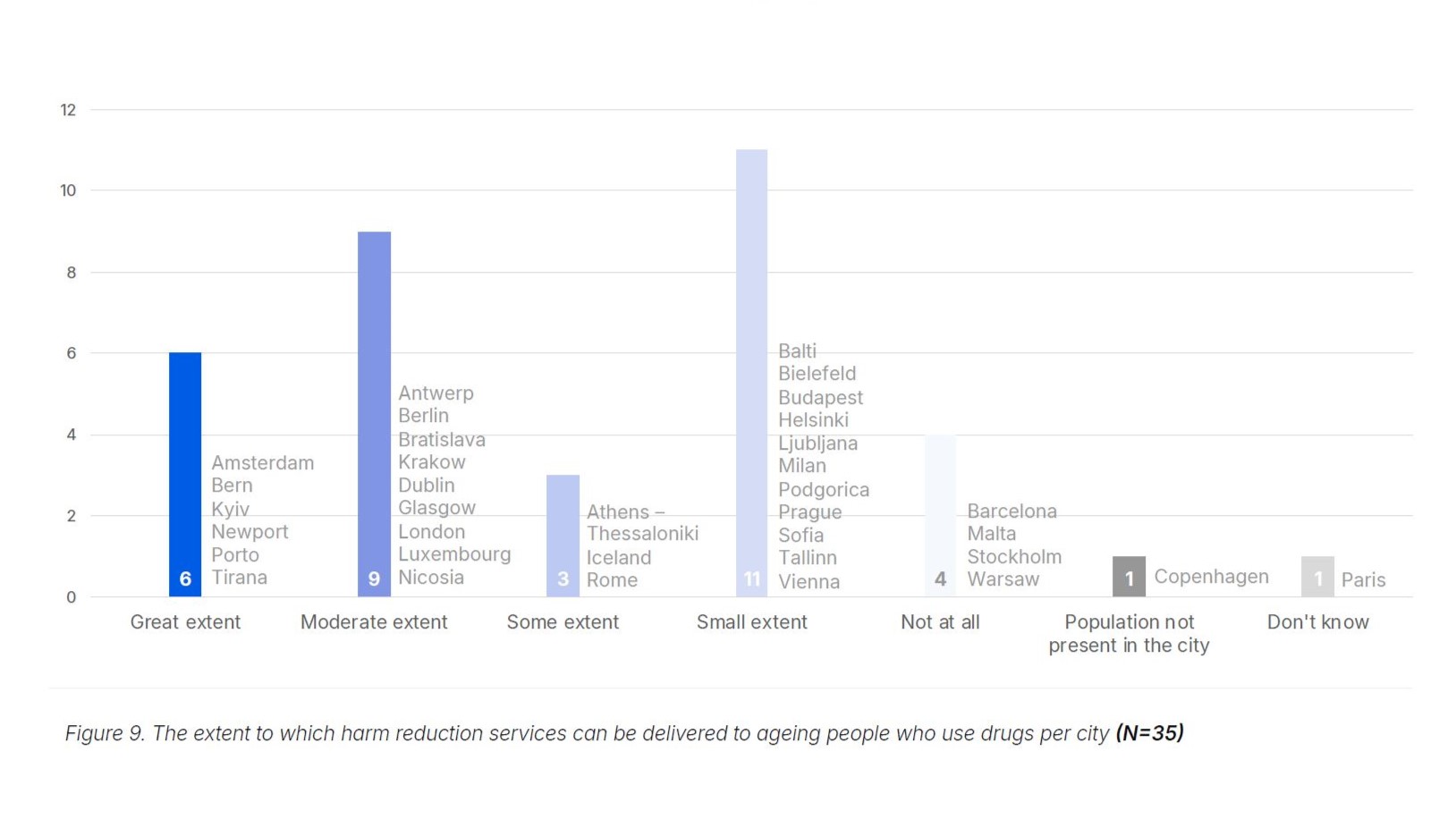
Would you pick one graph that you find significant and explain why it is relevant?
All of them are significant in their own way. What I would suggest is Figure 9 on service delivery for ageing people who use drugs, a category that we introduced last year. Ageing people who use drugs are becoming a more and more significant group among the clients of harm reduction services all over Europe. The people for whom the first harm reduction services were established in the 1980s are ageing, and there is an increasingly recognised need for developing and adjusting services to their needs, which significantly differ from those of the other subgroups, and there hasn’t been sufficient focus on them so far.